What is a herniated disc?
There are 33 vertebrae in your spine and 23 intervertebral discs which are located between each of the cervical, thoracic and lumbar vertebrae. These flat, thin discs serve as shock absorbers for your spine. Your intervertebral discs are incredibly sturdy, but they can weaken with age and may herniate. When they do, you may experience slight back pain which worsens with time, and can become quite painful.
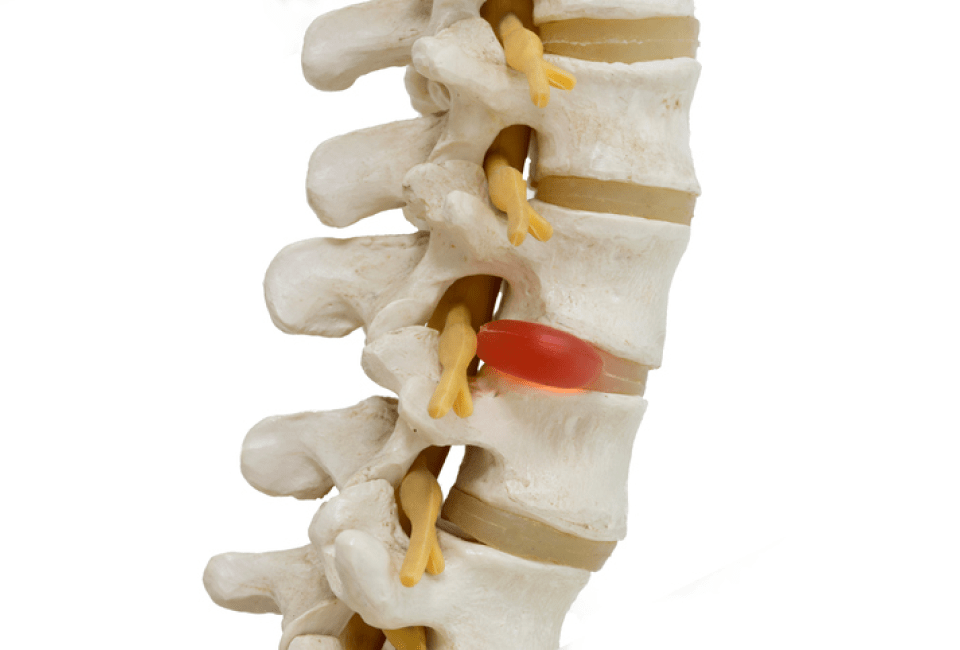
When the outer section of the disc is weakened or worn down, it can tear open or herniate which allows the soft center of the disc, the nucleus pulposus, to leak through the rigid outer fibers (annulus fibrosis). Less typically, failure in the annulus fibrosis can be the source for the herniation. The material that is extruded from the disc can compress neurons adjacent to the disc and cause pain.
In one study of herniated discs, extruded tissue from the soft center of the disc accounted for 29% of the cases. Only 13% of the herniated discs studied were traced back to the annulus fibrosus, the outer part of the disc (1). If the herniated disc is located in the upper spine (cervical), you may experience radiating pain in your fingers, arms and shoulders. If the disc herniation is in the lower spine (lumbar) patients may experience tingling pain in their feet, legs, hips and buttocks. This type of radiating pain is called radiculopathy. Over 90% of disc herniations are lumbar-based (2).
Herniated Discs Overview Video
How common is a herniated disc?
In the US, twenty-eight percent of people over forty will experience a disc abnormality. A herniated disc can occur in any intervertebral disc on your spine, but most commonly they are found in your lower (lumbar) spine. Generally, the disc is weakened with time. We all suffer a certain degree of spinal degeneration, and typically the condition may start slowly with a slight back pain that worsens gradually. However, physical exertion like pushing a car out of a snowdrift in the Sierras, helping someone move, or just swinging a golf club the wrong way can cause a herniation. What is even more perplexing is that there are many cases of herniated discs that cause no pain. Men are twice as likely to have a herniated disc than females (3). The average age for individuals to suffer from a herniated disc is about 43-years old with only rare instances occurring in children and teens.
How is a herniated disc diagnosed?
The symptoms of a herniated disc depend on their location along the spine. If you feel twinges of pain in your neck or between your shoulder blades, tingling sensations or even numbness along your arms to your fingers, you may have herniated disc in your upper spine. You may also experience pangs of pain when you turn your head.
If you are experiencing pain in your lower back or feel like a tingling along your hips, buttocks, and down your legs to your feet, there is a good chance that you have a herniated disc in your lower back.
Diagnosing the root cause of your herniated disc requires a full patient history, clearly defined pain symptoms and a series of physical tests that will help your doctor locate the herniated disc. You may be asked to lie down and raise your legs and perform exercises that help correlate the type of pain you are feeling with a probable location in your spine. Your doctor may test your walking gait, posture, muscle strength and your reflexes. During this stage, your doctor will check to see if the pain is referred or related to cauda equina syndrome.
Generally, the physical exams will identify the cause of the pain. The good news is that most herniated discs do not require surgery. Your doctor may request X-rays which will help rule out tumors and fractures and provide a good overview of the health of your spine. CT scans, MRIs and Myelograms are used if there is uncertainty about the pain source.
What are the treatments for a herniated disc?
To treat a herniated disc, your doctor may suggest a conservative, ‘wait and see’ approach using over the counter medications like Advil or opioid-based pain relievers.
Dr. Melamed takes a proactive, patient-centered perspective that steers clear of any opioid-based pain relievers. He may suggest holistic treatments based on integrative medicine that takes into account the whole person with a focus on lifestyle. He may recommend alternative conservative treatments like physical therapy, chiropractic sessions, acupuncture, yoga, and even a healthier diet. If you are a smoker, Dr. Melamed can help you kick your habit, especially if you are serious about eliminating your back pain.
If after four to six weeks, the conservative treatments are not getting anywhere, and your pain continues, or the size of the disc herniation is above average, or you are experiencing bladder or bowel control, then surgery may be your best option.
One of the most common surgeries for a herniated disc is lumbar microdiscectomy which is a minimally invasive procedure that decompresses nerve pathways by removing a small part of the herniated portion of the disc that is pressing on them. Due to the small incision and the benign treatment of the back muscles, pain and infection are reduced. The procedure can be performed in Dr. Melamed’s clinic over a few hours with the patient returning home the same day. Dr. Melamed’s technique does not require the use of opioid-based pain relievers during or after the surgery. This significantly eliminates the risk of developing an opioid addiction. Back pain relief is almost immediate, and the microsurgical technique has an excellent success record of 84% (4).
Click on the “Make An Appointment” button at the top of this page, or call Dr. Melamed’s office for more information. This is a great day to deal with your back pain. Call us at 424-21-SPINE.
References:
1: Lumbar Disc Herniation, Franco Postacchini, Pg. 157, Springer Science Library
2: Ibid., Pg. 152
3: Ibid, Pg. 152
4: Dohrmann GJ, Mansour N. Long-Term Results of Various Operations for Lumbar Disc Herniation: Analysis of over 39,000 Patients. Med Princ Pract. 2015;24(3):285-90